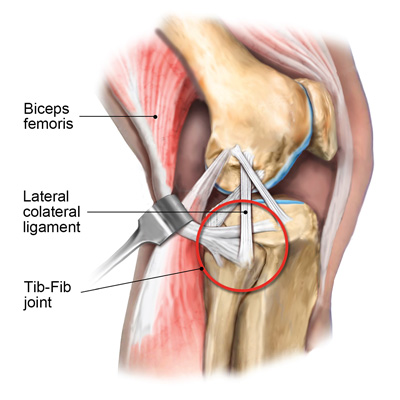
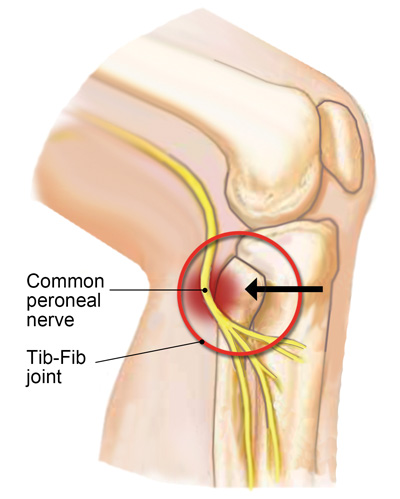
One of the primary functions of the tib-fib synovial joint is to help dissipate lower leg torsional stresses during gait. When the knee is extended, the biceps femoris, popliteus, and lateral collateral ligaments provide good joint stability, but with the knee flexed, these connective tissues lose much of their supportive capability. That’s one reason tib-fib injuries are most often seen in sports that involve twisting forces around the knee and ankle, such as football, wrestling, soccer, judo, gymnastics, long jumping, and skiing.
In my non-athletic clients, tib-fib problems typically arise from overuse injuries on jobs that require repetitive activities. Clinically, I’ve found many clients presenting with lateral tib-fib pain from overuse also have an underlying body structure deficit, such as overpronated feet and valgus knees. In these cases, forces accumulate that cannot be properly dissipated or, worse yet, may be misdirected into areas not intended to handle the load, as we will see in the case study presented later in this article.
Common signs and symptoms of tib-fib dysfunction:
- Pain with one-legged weight bearing
- Outer knee pain aggravated by direct pressure to the fibular head
- Limited knee extension
- Crepitus (grinding) during knee movement
- Visible deformity
- Ankle movements that provoke lateral knee pain
Palpation and Assessment
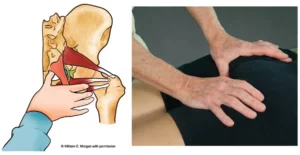
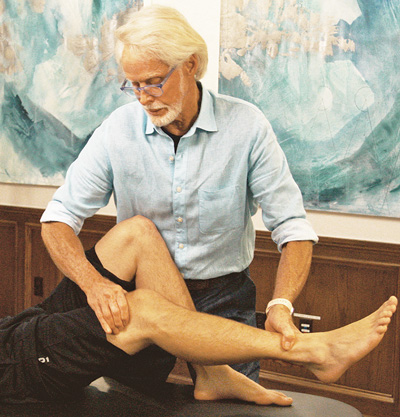
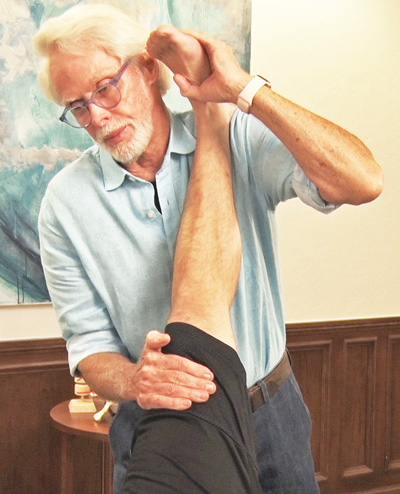
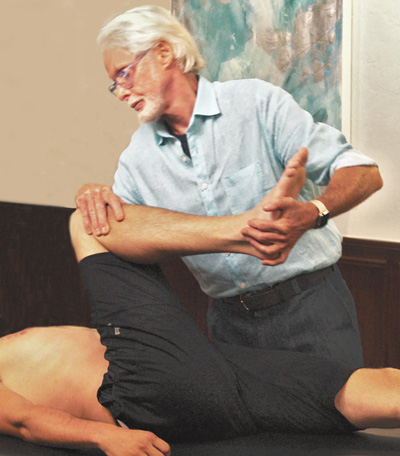
Yale University researcher Dr. John Ogden was the first to conduct studies evaluating the anteroposterior (A-P) motion of the proximal fibula and correlating it with positional changes of the knee.1 He found that when the knee flexes, the proximal fibular head moves anteriorly, and during knee extension, the fibula translates posteriorly (approximately one centimeter in both directions). In Image 2. , I demonstrate an assessment version of Ogden’s A-P glide on my client Keith’s right knee.
Keith’s Case Study
When assessing Keith’s A-P glide, I noticed a restriction to anterior translation of fibula on tibia accompanied by tenderness and a slight grinding noise. I recalled that during Keith’s history intake he described a pretty significant inversion ankle sprain and hamstring contusion experienced during a judo fall that left him with a temporary limp, intermittent lateral knee pain, and lower leg numbness.
Summary
If you have a client with knee pain that fits some of the patterns outlined above, the tib-fib may be involved. In such cases, the first order of business is to determine the type and degree of tissue damage based on history, assessment, and clinical reasoning. Left untreated, tib-fib fixations can cause long-term difficulties including pain, gait disturbance, and inferior sports performance. Hopefully, a better understanding of this often-neglected joint leads to less clinical error and improved client outcomes.
References
1. Ogden, J.A. (1974). Subluxation and dislocation of the proximal tibiofibular joint. Journal of Bone & Joint Surgery, 56(1), 145-154.
On sale this week only!
Save 25% off the "Dalton Technique Treasures" eCourse
The “Dalton Technique Treasures” eLearning course is a compilation of some of Erik’s favorite Myoskeletal Alignment Techniques (MAT). Learn MAT techniques to assess and address specific sports injuries, structural misalignment, nervous system overload, and overuse conditions. ON SALE UNTIL April 29th! Get Lifetime Access: As in all our eLearning courses, you get easy access to the course online and there is no expiry date.