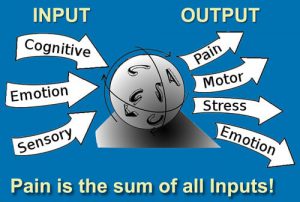
When the brain senses bony instability or tissue damage in-and-around the spine, information is compiled and ‘fast-tracked’ to the brain where a determination is made as to the degree of threat and appropriate action required (Fig. 1). Layering the area with protective muscle guarding is a common decision handed down by the cortex when joint lesions threaten central nervous system functioning. Protective spasm is the brain’s reflexogenic attempt to prevent further insult to injured tissues. By splinting the area with spasm, muscle ‘locking’ effectively reduces painful joint movements. The brain’s motto: “If in doubt, lock it out.” For the manual therapist, this is a time for critical thinking and challenging decision making. We must ask ourselves: 1) what happens if I attempt to release this spasm, 2) should I be elbowing the myofascia that’s compressing the joint, and, 3) could my deep tissue treatment be creating greater instability and initiating more low back pain? Muscle knots are not all created equal…if they keep coming back; maybe they’re supposed to be there.
Today’s bodyworker will always be confronted with the mysteries of muscle guarding, so we must revisit current treatment strategies while seeking new ways to deal with the underlying causes of this problematic condition. Here’s a recent case demonstrating one type of spasm where poor intrinsic / extrinsic muscle balance created joint jamming which, in turn, triggered secondary muscle guarding.
Case Study
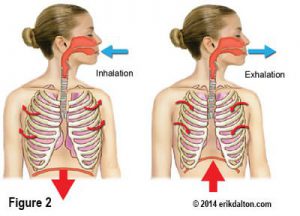
Kate came in complaining of ‘stabbing’ right-sided back spasm while leaning over to pick up her toddler (Fig. 2). Gait analysis and movement screening tests indicated significant length/strength torso imbalance and poor global and local muscle activation. Because Kate’s job required her to sit hours-on-end at a main-frame Hertz computer terminal, faulty ingrained movement patterns from the flexed posture may have finally caught up with her during the forward bending and twisting incident. Surprisingly, her hip capsule mobility, SI joint stability and rib cage mobility tested fine and did not seem to be contributing to the low back spasm.
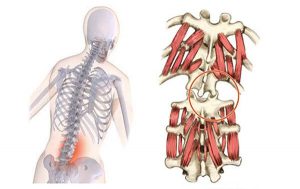
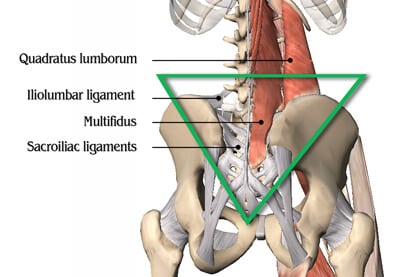
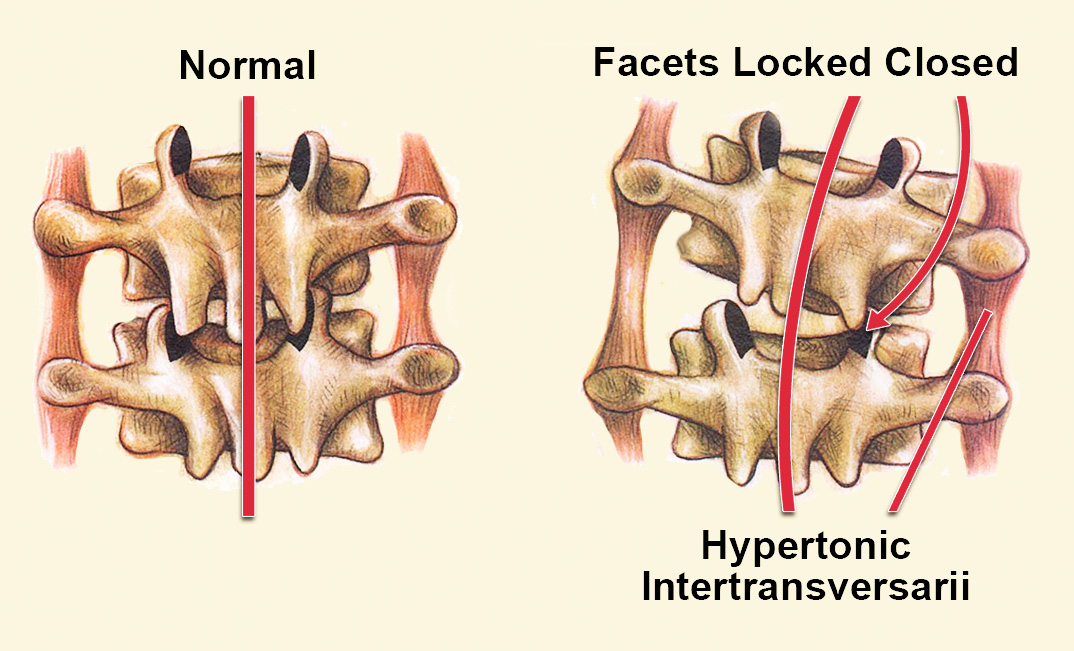
But when the trunk’s antigravity fascial support system fails, too much weight descends on spine-related tissues (Fig. 3) Joint capsules, discs, spinal ligaments, facets and transversospinalis muscles must possess both mobility and stability while constantly providing proprioceptive feedback to the cord and brain. In Kate’s case, asymmetrical loading and twisting of the torso during forward bending prevented the L4 facets from opening on L5 on the right side (Fig. 4). The subsequent loss of joint-play created palpable inhibition (atrophy) of the multifidus muscle on the side of the joint blockage. But, just lateral to the jammed joints was a visible and palpable ‘big wad’ of unyielding lumbar erector spasm that had been living there for weeks.
To help calm the agitated mechanoreceptors and restore multifidus tone, the motion-restricted facet joints had to be manually disengaged. With Kate lying on her left side, she slowly began flexing and relaxing her right knee-to-chest while my thumbs gently applied anterior/superior pressure in the groove at L4 (Fig. 5). Once the joint capsule, rotatores, and spinal ligament fibrosis began to melt, the adhesive facets released and I could feel the erector spasm settle down. The focus then shifted to fascial balancing work to hydrate adhesive tissue residue left behind from the spasm. Nerve Mobilization techniques are excellent for freeing fixated tissues in the lamina groove but in Myoskeletal Therapy® we use articular stretching techniques (AST) described above. AST is applied with fingers, thumbs and elbows to loosen joint capsules, fibrotic ligaments, groove muscles and fixated facets.
As the muscle gently tugs on the bony attachment stabilized by the clinician, one vertebra moves in relation to its counterpart. After a few sessions, the pain, spasm and sympathetic postural distortions usually self-correct at they did with Kate. Once Kate’s spine and paravertebral fascia regained free-floating mobility, she was referred for functional training to normalize length/strength balance and restore proper muscle activation patterns.

On sale this week only!
Save 25% off the Posture Pain Performance course!
NEW! USB version with enhanced video
Discover the foundational principles behind MAT technique as we take you on an in-depth look at the connection between pain, posture and function. Save 25% off the Posture Pain Performance course this week only. Offer expires Monday April 22nd. Click the button below for more information and to purchase the course. Upon completion receive 20CE hours and a certificate of completion to display in your office.
Bonus: Order the Home Study version and receive the e-Course for FREE!