It was a moment of epiphany, where wisdom hung heavily in the air. The legendary, feisty, 92-year-old Detroit osteopath Clarence Harvey was about to share his unusual but profound mantra for assessing neck-and-back dysfunction with a classroom packed with students. Wearing a slight smile on his wizened face, he slowly turned to the chalkboard and boldly wrote in large letters, “Don’t chase the pain.” Although initially the intent of his statement seemed vague and somewhat cloudy, it stirred memories dating back 20 years, when the queen of fascial work, Ida Rolf, Ph.D., made a strikingly similar comment that supported Harvey ‘s advice. During an Esalen Institute presentation I attended in the early ’70s, she had bluntly stated, “Get ’em aligned and balanced. If the pain goes away, that’s their tough luck.”
Years of clinical experience had apparently brought these two manual-therapy legends to the same conclusion. Since neck/back dysfunction typically involves many pain producing structures and referral patterns, simply chasing the pain by addressing clients’ bodies where they hurt is, at best, a temporary quick-fix. Both Harvey and Rolf agreed that trying to decide exactly which structures are causing client’s neck and low back pain was basically a waste of time.
Although muscles are partly to blame, advanced diagnostic equipment confirms their theories as new research implicates other pain generating soft tissues, such as:
- Ligaments
- Discs
- Nerve dura
- Fascia
- Joint capsules
Previously thought of as only mechanical structures, clinical researchers today substantiate the presence of neural innervation in all these soft tissues.
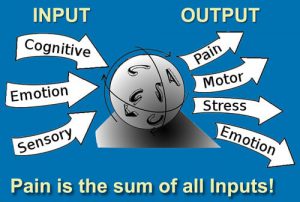
Holistic alleviation of pain is largely dependent on restoration of proper body alignment, range of motion and proprioception. According to the great biomedical researcher Nikolai Bogduk, M.D., “Pain upon movement is not a criteria from which a biomechanical assessment can be made. To reach an accurate assessment, we need to evaluate function according to a dynamic structural model.” As massage therapists learn to integrate alignment techniques into their clinical practices, clients’ aches and pains begin to disappear without the therapist ever having to know exactly which of the soft tissues caused the pain. The trick is developing a simple and effective structural model that is easily adaptable to a typical massage therapy pain management session.
Eight Procedures
By incorporating a wide assortment of new and old manual therapy modalities, the Myoskeletal Alignment Techniques (MAT) method helps manage the neck/back pain puzzle by addressing all soft-tissue back structures in one formula.
Massage therapists trained in the MAT method of deep tissue therapy find success in assessing and correcting a wide range of chronic pain conditions by integrating the following eight procedures:
- Observe for lower and upper crossed syndromes upon the client’s entrance
- Conduct a five-minute structural assessment on the therapy table with the client draped
- Lengthen short, hypertonic muscles with deep-tissue, myofascial release and assisted-stretching techniques
- Tone weak, inhibited muscles with fast-paced spindle-stimulating maneuvers
- Fibroblast-friction hypermobile ligaments and loosen hypomobile ligaments using finger, fist and elbow procedures
- Massage fibrotic transversospinalis muscles to unlock stuck facet joints or to stimulate spindles if weak and inhibited
- Restore joint play and capsular flexibility with co-activating receptor techniques
- Relieve disc compression and dural drag with gentle distraction maneuvers
Many of today’s rapidly evolving massage schools teach students various methods for visually assessing distorted postural patterns. Special attention is usually given to obvious anterior/posterior body asymmetries, such as forward-drawn heads, swayed backs and rounded shoulders.
One medical researcher in particular, Vladimer Janda, M.D., of Czechoslovakia , has been instrumental in advancing and simplifying this visual assessment model. Unfortunately, his 40-plus years as the world’s leading authority on the effects of muscle imbalances on posture has only recently been introduced to the audience that can most dearly benefit-the massage community.
Visual assessment made easy
Having had the good fortune to observe the brilliant work of Janda in 1992, my mission was clear: to immediately integrate this practical and timely information into the MAT method of assessment. Although Janda’s research concerning muscle imbalance patterns and neuromuscular firing order falls among the most valuable gifts presented to today’s clinical massage therapist, it has been sadly underutilized in most bodywork training.
In 1988 Janda surprised the biomedical community with a remarkable discovery: All striated muscles of the body respond to stress in different but predictable ways. Simply stated, certain muscles tighten while others weaken when exposed to the same stressors. Janda’s formula for predicting tight and weak muscle groups helps explain why so many clients present with the same aberrant postures. Investigators now believe these muscle imbalance patterns develop from a bombardment of abnormal neurologic information to the spinal cord and brain, due to tension, trauma, poor posture, joint blockage, genetic influences, excessive physical demands or habitual movement patterns.
Upper and Lower Crossed Syndromes
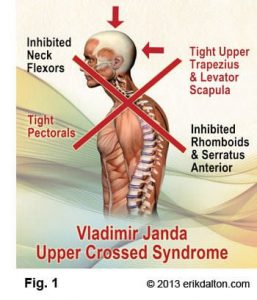
Today’s massage therapist should enjoy working with Janda’s upper and lower, or proximal-and-distal, crossed syndrome theory when dealing with clients who suffer from neck or back pain. According to Janda, when upper crossed muscles, such as the pectorals, upper trapezius, levator scapulae, latissimus dorsi, sternocleidomastoid, anterior scalenes, suboccipitals and subscapularis are stressed, they tighten and become neurologically facilitated.
This category of muscles was labeled tonic, or postural. Inversely, electromyographic studies found that other upper crossed muscles, such as the longus capitis, longus colli, hyoids, serratus anterior, posterior rotator cuff, rhomboid major and lower trapezius, actually weaken when exposed to the same stressors. This second set of muscles was labeled phasic, or dynamic. Amazingly, this muscular response occurs in consistent and predictable patterns regardless of the pathologic condition or the dysfunction present in the tested subjects.
Typical Muscle Imbalances in Upper Crossed Syndrome
Tight, Facilitated:
- Pectorals
- Upper Trapezius
- Levator Scapulae
- Sternocleidomastoid
- Anterior Scalenes
- Suboccipitals
- Subscapularis
- Latissimus
- Dorsi
Weak, Inhibited:
- Longus
- Capitis & Colli
- Hyoids
- Serratus Anterior
- Rhomboids
- Lower & Middle Trapezius
- Posterior Rotator Cuff
Typical Muscle Imbalances in the Lower Crossed Syndrome
Tight, Facilitated:
- Iliopsoas
- Rectus Femoris
- Hamstrings
- Lumbar Erectors
- Tensor Fascia Latae
- Thigh Adductors
- Piriformis
- Quadratus Lumborum
Weak, Inhibited:
- Rectus Abdominis
- Gluteals
- Vastus Medialis
- Vastus Lateralis
- Transversus Abdominis

The upper crossed syndrome. Notice how the tight line (a) passes through the levator scapulae, upper trapezius and the pectorals, causing shoulder elevation and scapular protraction. Inhibition in the deep neck flexors and lower shoulder stabilizers (b) permits this asymmetry.
Since the forward head is the most common postural fault seen in our society, Janda’s upper crossed illustration is extremely helpful in visualizing exactly which muscles pull unevenly to create this distorted posture. Notice in the upper crossed illustration how the tight line (a in Figure ) passes through the levator scapulae, upper trapezius and the pectorals. Sustained hypercontraction in these typically tonic muscles elevates and protracts the shoulders. Conversely, one can clearly see how the deep neck flexors and lower shoulder stabilizers that make up the weak line (b in figure) permit this asymmetry.
The lower crossed syndrome. The tight line (a) travels through the iliopsoas and lumbar erectors, which pull and hold this aberrant swayback posture. Reciprocal inhibition weakens the abdominals and gluteals (b) allowing this dysfunctional pattern to develop.
Janda employs the same concepts when analyzing the lower crossed problem. View how the tight line (a in Figure ) travels through the iliopsoas and lumbar erectors, while the weak line (b in Figure ) connects the lower abdominals and gluteals. In this crossed pattern, the short iliopsoas muscles anteriorly tilt the pelvis, creating excessive lumbar lordosis while erector spinae myofascial contractures hold this “bowing” pattern. The weak abdominals and gluteals, unable to stabilize the pelvis, allow this aberrant swayback pattern to develop. Still, a frustrating question remains: Why do so many clients present with this lower crossed pattern? The answer is, to me, painfully obvious: flexion addiction.
A Society of Flexion Addicts

The last century has witnessed a dramatic acceleration in our culture’s flexion addiction. This pervasive and insidious condition is primarily due to the population’s generational transition from an active group of movers to a sedentary bunch of sitters.
Davis’s Law emphasizes that if muscles are lax for extended periods of time, gamma gain and reciprocal inhibition will take up the slack. Thus is the case with the hip flexors. As the psoas and rectus femoris neurologically shorten from prolonged sitting, the ilia are pulled in an anterior/inferior direction, which results in excessive lumbar lordosis when standing. Compensations from this swayback condition often lead to thoracic hyperkyphosis, forward head postures and typical upper crossed asymmetries. Researchers estimate that up to 75 percent of chronic neck/back pain clients will present with one or both of these crossed patterns.
Consequently, any therapist’s practice benefits by utilizing Janda’s list of typically tight and weak muscles when addressing neck and low back pain complaints. The MAT method stresses that each pain management session begin with the intent of creating balance between the tight tonic and weak phasic muscle groups listed in Janda’s formula. The therapist begins by selecting a therapeutic technique to lengthen shortened, hypertonic muscles. Once length and flexibility have been restored to tight muscles and their fascia, specific fast-paced finger and fist techniques stimulate muscle spindles to tonify the weaker, inhibited groups. The therapist may choose a specific MAT maneuver to correct the asymmetries, or delve into his or her own toolbox for a familiar technique that has proven successful in the past. The MAT method emphasizes that specific technique selection is not as important as knowing why that particular muscle-release maneuver was chosen.
However, all hand, elbow, finger, fist and thumb techniques should correspond with the type of tissue manipulated. Tight, tonic muscles require restoration of extensibility, while weak phasics demand restoration of contractability. Incorporating Janda’s visual models of tonics and phasics makes structural work easy and fun. Of course, clients may present with occasional pattern reversals, such as military shoulders and flat backs. Prolonged slumping while sitting will eventually flatten or reverse the lumbar curve by overstretching posterior low-back ligaments. Hyperextension exercises, such as the hatha yoga cobra pose, are often helpful in reversing this painful postural pattern. Simple session modifications to Janda’s upper and lower cross formula will also restore function to clients experiencing loss of lumbar lordosis.
It should be noted that therapists frequently encounter side-to-side imbalances, such as a low shoulder, short leg or cocked head. These asymmetries are often the result of powerful unilateral myofascial forces tugging on the body’s bony framework, jamming spinal facet joints and irritating sensitive joint receptors. Facets are possibly the most innervated structures in the spine. Therefore, when the joint’s axis of rotation is disrupted due to myofascial shortening, the sensitive articular receptors provoke sympathetic spasm in neighboring muscles, causing the body to twist and torque in an effort at pain avoidance. As gravitational strain is added to the equation, unilateral distortions quickly become chronic pain-generators. So, how does the manual therapist know if these distorted postural patterns result from myofascial strains or joint dysfunction?
Tight Muscles or Joint Dysfunction?
As described in the first part of this series, Mobilizing Joints Through Muscle Manipulation (January/February), tight muscles create asymmetry and weak muscles permit asymmetry in both the myofascial and skeletal systems. Deep, intrinsic muscles and the body’s bony framework are inseparable: What affects one always affects the other. Until the therapist develops a basic understanding of how deep tissue techniques affect the bony framework, random deep tissue work is contraindicated. Massage therapists who commonly deal with chronic pain and postural problems profit by studying the laws of spinal biomechanics and learning to focus therapeutic intent on both myofascial and spine-related soft tissues.
A good example of how poor skeletal alignment promotes protective muscle spasm and aberrant postures is frequently encountered in clients suffering long-term neck, upper-shoulder and arm pain. People who habitually hold the telephone with one shoulder frequently develop chronic unilateral hypertonicity in the levator scapula and splenius cervicis muscles. Because of their common attachments at the top three or four cervical transverse processes, unilateral contraction of these muscles side-bends the neck and elevates the shoulder to help secure the phone. Problems escalate as the deep spinal rotators react to the unilateral sustained hypercontraction. When overstimulated, these fibrotic little muscles are notorious for locking facets closed on the ipsilateral side and open on the contralateral side.
Sensitive joint receptors respond to these sustained torsional forces by flooding the spinal cord with noxious afferent messages that tighten or weaken the little spinal rotator muscles, causing alterations in their firing order pattern. In scoliotic clients, therapists commonly palpate short/hypertonic rotators on the concave side and weak/inhibited muscles on the side of the convexity.
Repeated exposure to one-sided compressive forces from prolonged unilateral neck side-bending irritates the joint’s articular cartilages and promotes adhesive tissue build-up in cervicothoracic vertebrae and upper rib capsules. Because of the common attachments of the anterior scalenes with levator scapulae and splenius cervicis, unilateral sympathetic scalene spasm can join forces and pull the neck forward into an awkward flexed/side-bent/rotated position. Overstretched joint capsules soon fibrose and facet joints frequently become locked in an open position. The result: local neck ache or referred pain into the arm and interscapular area. Left unaddressed, the condition worsens.
Assume for a moment that the forward-head posture is subtly being pulled into right side-bending and right rotation due to combined hypercontraction in the levator and splenius cervicis muscles. As the client attempts to raise her head from a flexed to extended position, if the right T3 facet joint cartilage is swollen from prolonged right side-bending, it can get stuck and not be able to slide back in its proper closed position on T4. Because the left facets are operating smoothly, the superior facet on that side gladly slides closed during this maneuver. Unfortunately, because the T3 joint on the right is unable to close properly, it forces the T3-4 joint to rotate left, as illustrated below.

A swollen right facet at T3 is unable to close during extension efforts by the client, causing the vertebra to rotate left.
The dysfunctional facet joint capsule will soon fibrose, locking T-3 left rotated. To compensate, the T3 rib on the side that is not closing is usually forced into internal rotation. Now the nagging pain begins. Prolonged irritation allows this “dynamic duo” (vertebra/rib fixation) to feed off each other, creating reflexogenic inhibition in the surrounding paravertebral muscles, including the rhomboids and trapezius muscles. Retraining exercises to strengthen the lower shoulder stabilizer muscles to help resist the powerful pull of the massive pectorals are useless until both these joint fixations are addressed. Second only to backward sacral torsions, vertebra/rib dysfunction is probably the longest-lasting and most irritating joint-related problem a client will ever experience.
A Sample MAT Joint-Release Routine
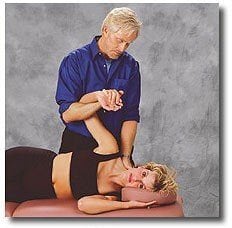
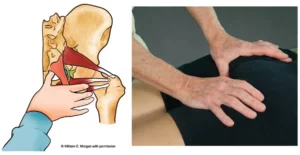
To remedy this distressful situation, the splenius cervicis, levator scapula and anterior scalenes on the right must first be lengthened.
- The therapist lengthens the splenius cervicis, levator scapula and scalenes by pinning the attachments with his or her left hand, while mobilizing the shoulder girdle with a right-arm lock
- Since the T3-4 joint is rotated left, the therapist will feel a hard or “stringy” knot on the client’s left side in the spinal groove when palpating that area
- With the client in a prone position, the therapist’s fingers or thumbs start by loosening the overlying myofascia and digging out adhesions in the deep spinal rotator muscles
- Soon a bony knot will be palpated on the left at T-3, indicating the vertebra has, indeed, rotated left
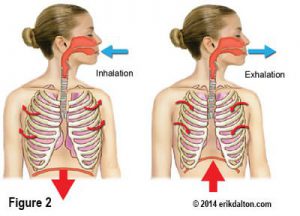
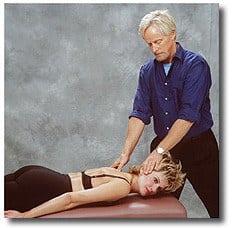
The therapist’s right thumb is placed on the protruding left transverse process while the left hand lightly rests on the back of the client’s neck. Using gentle, sustained anterior pressure on the bony knot, the client is instructed to inhale to a count of five, while carefully attempting to extend and right-rotate her head against the sustained isometric resistance from the therapist’s left hand.
As the bony knot pushes back against the therapist’s resistant thumb, a strong Golgi tendon organ release is transferred through the transverse process to the adjoining spinal rotator muscles, creating increased capsular flexibility and subsequent joint decompression.
As the client exhales and relaxes, a post-isometric relaxation response further softens the muscles and joint capsule, allowing the therapist’s thumb to slowly de-rotate and release the fixation at T3-4.
Gentle thumb pressure combined with extension and right rotation efforts by the client encourage the stuck right facet to slide down into its proper position. Fortunately, the internally rotated rib on the opposite side frequently fixes itself as the dysfunctional facet comes into alignment.
If immediate softening is palpated in the surrounding spinal muscles following this, then the therapist has done her or his job. Always check to see if the rib on the right has corrected itself by lightly scanning the rib shafts with soft fingertips, inferior to superior, feeling for a bump at about T3. If a slightly bulging rib shaft is palpated, the rib is still stuck in internal rotation. With fingers or thumbs, simply release the intercostal muscles above the dysfunctional rib in a medial to lateral direction. Then apply the same basic procedure as above to align the costotransverse rib joint.
In Summary
- The therapist contacts the client’s left T3 transverse process with the therapist’s right thumb while his or her left hand gently rests on the client’s neck
- With a 10-percent effort, the client inhales while extending and right rotating her head against isometric resistance from the therapist’s left hand
- As T3 attempts to rotate left, the therapist’s right thumb resists this effort, causing a Golgi tendon relaxation response in the fibrotic tissues that are restricting closure of the joint
Pain Free Clients
Many years have passed since the gifts of two great and gifted visionaries-Ida Rolf, Ph.D., and Vladimer Janda, M.D.-were bestowed on me. Every day I become more convinced that managing the pain is simply an elusive journey that sidetracks us into addressing obvious problems, while missing the real cause of our clients’ dysfunction. By focusing infinitely on the body’s complex systems of interconnecting networks, one can become lost in the minutiae without appreciating our built-in, self-sustaining system that thrives when the effects of gravitational strain are reduced by proper alignment. The old adage, “You can’t see the forest for the trees,” drives home the idea of embracing the natural order of balance and simplicity within the cinemascopic context of its overall complexity.
By integrating the technological advancements of today with the wisdom passed on from our forefathers and foremothers, we can achieve the success we desire: pain-free, mobile and fully functioning clients.
References
- Bogduk, N: “Pathology of Lumbar Disc Pain,” Journal of Manual Medicine, 1990.
Please note: This article and the accompanying graphics are not a substitute for hands-on training. Readers are urged to seek training and/or to self-assess to make sure they have sufficient education and experience to understand the information presented here and to safely perform the techniques described.
On sale this week only!
Save 25% off the "Dalton Technique Treasures" eCourse
The “Dalton Technique Treasures” eLearning course is a compilation of some of Erik’s favorite Myoskeletal Alignment Techniques (MAT). Learn MAT techniques to assess and address specific sports injuries, structural misalignment, nervous system overload, and overuse conditions. ON SALE UNTIL April 29th! Get Lifetime Access: As in all our eLearning courses, you get easy access to the course online and there is no expiry date.